Yes, Aetna may cover skin removal after weight loss. Coverage depends on specific criteria.
After a significant weight loss, many people face excess skin. This can cause discomfort, infections, and emotional distress. Skin removal surgery can help, but it’s expensive. If you have Aetna insurance, you might wonder if they cover this procedure. Insurance coverage for skin removal often depends on medical necessity.
Aetna might cover it if the excess skin causes health problems. Understanding Aetna’s criteria and process is key to knowing if you qualify. In this post, we will explore the details of Aetna’s coverage for skin removal after weight loss. Keep reading to find out what you need to know before moving forward with your plans.

Credit: www.ljcsc.com
Introduction To Skin Removal Surgery
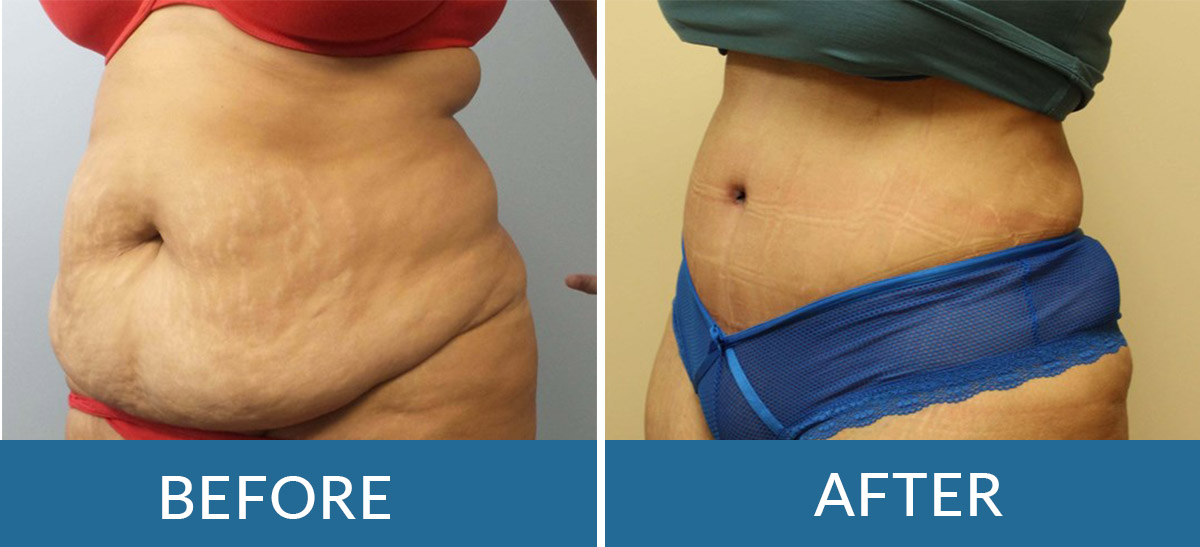
Skin removal surgery helps people who have lost a lot of weight. This weight loss can leave extra, loose skin. The extra skin can cause problems. It can rub and lead to rashes or infections. People might feel self-conscious about their appearance.
There are several common procedures for skin removal. A tummy tuck removes skin from the belly. Arm lifts help tighten the skin on the arms. Thigh lifts focus on the legs. Body lifts can remove skin from many areas at once.
Aetna Insurance Overview
Aetna offers many health insurance plans. These include HMO, PPO, and POS. Each plan has unique features. HMO plans usually require you to choose a primary care doctor. PPO plans offer more flexibility. POS plans mix features of both HMO and PPO.
Understanding what your plan covers is key. Skin removal after weight loss is often seen as cosmetic surgery. Many plans do not cover cosmetic procedures. Some plans might cover if it’s medically necessary. Check your policy for details. Always consult with your insurance provider.
Criteria For Coverage
Aetna may cover skin removal if it is medically necessary. The skin must cause problems. Problems like infections or sores. A doctor must check the skin. The doctor will decide if removal is needed.
Aetna does not cover skin removal for cosmetic reasons. If the skin is just loose but healthy, it is not covered. The doctor’s report is important. It must show why the surgery is needed.
Proper documents are needed for coverage. First, a doctor’s letter. This letter must explain why the skin removal is needed. Next, medical records. These records must show past treatments and problems. Photos may also be needed. Photos of the skin issues can help. All documents must be clear and complete.
Credit: bssny.com
Pre-approval Process
Aetna may cover skin removal after weight loss if it is medically necessary. The pre-approval process requires documentation from your doctor.
Initial Consultation
Aetna requires an initial consultation with a licensed doctor. The doctor will evaluate your need for skin removal. They check if the skin causes problems like infections. They also look for issues with mobility.
Submitting A Request
After the consultation, the doctor submits a request to Aetna. This request includes medical records and photos. It shows why the surgery is needed. The request must prove that the surgery is not just for looks. It needs to show medical necessity.
Commonly Covered Procedures
Panniculectomy is often covered by Aetna. This procedure removes the hanging skin from the lower belly. It can help reduce rashes and infections. The surgery can improve hygiene and comfort. Coverage depends on medical necessity.
Body lift surgery is sometimes covered by Aetna. This procedure tightens loose skin on the body. It can include the abdomen, buttocks, and thighs. The goal is to improve appearance and function. Medical necessity is key for coverage.
What To Do If Denied
Denied coverage for skin removal by Aetna? Appeal the decision with supporting medical documents. Consult your doctor for further advice.
Appeal Process
Receiving a denial can be frustrating. Always check the denial letter for reasons. Gather all necessary medical records and doctor notes. Submit an appeal to Aetna with these documents. State clearly why you need the surgery. Highlight health issues caused by excess skin. Follow up regularly on the status of your appeal. Be persistent and do not give up easily.
Alternative Options
If your appeal is denied, consider other options. Look into medical loans or payment plans. Some charities might help with funding. Discuss with your doctor about less expensive alternatives. Explore if other insurance plans offer better coverage. Seek support groups for advice and shared experiences. You are not alone in this journey.
Patient Testimonials
Many patients have shared their positive experiences with Aetna covering skin removal. John lost 100 pounds and had excess skin. Aetna covered his surgery, and he feels great now. Sarah also shared her story. She lost 150 pounds. Her surgery was covered too. She is now confident and happy.
Some patients faced delays and denials. It was hard for them. Lisa had to submit many documents. She was patient. After months, her surgery was approved. Mark faced a denial first. He appealed and finally got approval. These stories show it can be challenging. But persistence can help.
Tips For Navigating Insurance
Your doctor can help with insurance. They know what is needed. Ask for their help with documents. Provide medical records showing your need. Photos can show the excess skin. Doctor’s notes are very important. Keep talking with your doctor. Follow their advice closely. This can improve your chances.
Read your policy carefully. Know what is covered and what is not. Call Aetna to ask questions. Keep notes of your calls. Save all letters from Aetna. Stay organized with your papers. Ask for help if confused. Stay informed about your case. This can help you a lot.

Credit: jetmedicaltourism.com
Frequently Asked Questions
Does Aetna Cover Skin Removal Surgery?
Aetna may cover skin removal surgery if it is medically necessary. Approval depends on meeting specific criteria.
What Are The Requirements For Aetna To Cover Skin Removal?
Aetna requires documented medical necessity for skin removal. This includes issues like infections or physical limitations.
How Do I Get Aetna To Approve Skin Removal?
To get Aetna’s approval, provide detailed medical records. Include documentation of health issues caused by excess skin.
Is Skin Removal After Weight Loss Considered Cosmetic By Aetna?
Aetna often considers skin removal cosmetic, unless it’s proven medically necessary. Medical necessity must be clearly documented.
Conclusion
Understanding Aetna’s coverage for skin removal after weight loss is crucial. Always review your policy details carefully. Speak with your doctor about your options. They can provide guidance on necessary procedures. Contact Aetna for specific coverage questions. Clear communication helps you navigate insurance complexities.
Your well-being matters most. Make informed decisions. Stay proactive in your health journey.


